The Distinction Drawn Between ‘Mental’ and ‘Bodily’ Forms of Illness
- Rebecca Ivory

- Jan 8, 2023
- 10 min read
Updated: Mar 3, 2023
It is not unusual to think of the mind and body as two separate entities. The link between mental and physical health is complex and often misunderstood as such, and a distinction has long been drawn between the two ‘forms’ of illness (Kendell, 2001) due to—and because of—differences in how they are perceived, treated, diagnosed, and researched (broadly). Naturally, one might presume that mental and bodily forms of illness are distinct. The two kinds of illness have very different histories for example, not to mention the fact that both mental health awareness and services are only a recent phenomenon that are still unrecognised and/or stigmatised by many.
Despite appearances, is there a genuine and clear cut distinction to be drawn in the first place? What does it mean to draw a distinction, and is it feasible to draw a distinction between mental and bodily forms of illness so readily and naturally? This article will open up these very complex questions, investigating a phenomenological approach to the matter also.
Why Consider Taking a Phenomenological Approach?
Firstly, it’s worth exploring how phenomenology could provide an enhanced understanding of the experience of illness. Phenomenology, discussed at great length later, potentially undermines the idea of drawing a distinction between mental and bodily forms of illness – particularly when psychiatric disorders have remarkably bodily/physical features. Oftentimes the mind and body in fact work together to constitute wellbeing (Tang, 2017) or both are affected in illness (unlike what a distinction might suggest), as phenomenology reveals (Fuchs, 2013). This article will thus investigate the phenomenological ability to understand the distinction drawn between mental and bodily forms of illness, in particular with reference to (severe cases of) depression. Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (‘CFS/ME’) will also be considered. CFS/ME is an especially controversial and misunderstood illness, providing a good example of the severity of an unagreed upon or faulty distinction drawn between mental and bodily forms of illness (thus reflecting the importance of investigating the distinction).

The Distinction
Whilst there is a more concrete biological understanding available for ‘bodily’ illnesses, as reflected by the mechanical tests that diagnose patients, the same is not true of mental disorders. Mechanical tests unfortunately cannot confirm diagnoses for mental disorders, which are given based on the (informed) opinion of a clinician (First et al., 2014). The two kinds of illnesses prima facie appear quite dissimilar in this sense, for a multitude of reasons. This distinction, however, is a great deal more complicated than it first seems.
The distinction drawn between bodily and mental forms of illness is maintained by many groups which overall have a real influence on how anyone might perceive either type of illness, including its aetiology, severity, and treatment protocol. Various groups might include philosophers and theoretical thinkers, clinicians in practice, or the general public (to name some examples). These different groups notably maintain a distinction for different reasons, whether it be for pragmatic purposes, based on a natural assumption, or a metaphysical distinction. All are influenced by one another. The view of theoretical psychiatrists, for example, influences how the Diagnostic and Statistical Manual of Mental Disorders (‘DSM’) (American Psychiatric Association, 2013) is revised, and the DSM categories in turn influence clinical practice and funding for research and treatment. Finally, clinical practice then influences the perspectives of the general public, which is significant in that this alone goes full cycle and fuels all of the above views. (Societal/cultural views and stigma are important here, but notably deserve attention elsewhere).
This article is not by any means suggesting that mental and physical phenomena are not different in various ways, but that forms of each kind of illness are not often just ‘mental’ or just ‘bodily’. Drawing a distinction is an intricate, confusing, and possibly damaging business, even though the ‘mind’ and ‘body’ work together.
‘Bodily’ Illnesses
Why is a ‘bodily’ illness intuitively different to that of ill ‘mental’ health? Take a brief example, namely a genetic condition like Cystic Fibrosis (hereafter, ‘CF’), commonly understood as an illness of the body. Firstly, broadly speaking, it is known that the gene effected by CF controls the movement of salt and water in and out of cells (Davis, 2006). Secondly, it is also known that CF sufferers experience a build-up of thick sticky mucus in the lungs, digestive system and other organs, causing a variety of symptoms affecting the entire body (ibid). Such knowledge means that it is relatively straightforward to go on to diagnose CF. There are three types of screening now used: carrier testing, new-born screening, and antenatal testing (ibid.) CF is thus treatable via medication, physiotherapy, and transplants (ibid). CF could be understood as psychological in some respects, insofar as it makes sufferers feel miserable. This of course does not mean that CF is a ‘psychological’ or ‘mental’ illness, however. It is instead understood to be a bodily illness which may often—understandably—result in distressing psychological side effects.
‘Mental’ Illnesses
Take a contrasting example: the system for understanding, diagnosing, and treating ‘mental’ illnesses. First, there is not any concrete understanding—on the same kind of detectable biological level—of mental health problems. A good example (of many) is bipolar disorder (‘BD’). Also known as Bipolar Affective Disorder, this is a mood disorder. It causes the mood to swing from an extreme high to an extreme low, and includes manic symptoms such as increased energy, excitement, impulsive behaviour, and agitation (American Psychiatric Association, 2013). Depressive symptoms and psychotic symptoms can also occur, falling under the different types of the disorder. Unlike CF, however, causes are unknown. It is thought to be a combination of genetic and environmental factors and treated with medication and/or talking therapies (Leahy, 2007). Notably, however, the diagnosis and general understanding is not as straightforward (for instance, lack of mechanical tests available to make diagnoses. Also, observing symptoms is entirely different too).

Importantly, it is also merely thought that BD could be linked to genetics since it seems to run in families. Researchers have not found the exact genes that cause BD, and no single gene is responsible for BD (Leahy, 2007) (recall how a bodily illness like CF is known to be a genetic condition – the gene effected controls movement of water and salt in and out of cells). Since different chemicals in the brain affect mood and behaviour, too much or too little of these chemicals could mean one develops mania or depression, possibly accounting for BD (Leahy, 2007). Yet again, there is only minimal evidence for this to be the exact cause of BD. Most likely, it is thought that BD (like many mental disorders) is a ‘cocktail’ of factors, unlike specific or hard detectable biological evidence for many bodily illnesses on balance. This difference in current ability to understand each type of illness could be part of the reason why one draws a distinction between the two. It’s essentially a pragmatic distinction in this sense too, for example if health care services are divided up into physical and mental practices (like in the UK) (Hardy and Thomas, 2012).
CF and BD are notably very broad—but nevertheless appropriate—examples of why mental and bodily illnesses are often understood to be distinct. Mental illnesses, unlike many somatic illnesses, often have particularly complex and misunderstood aetiology thus requiring a very different approach to that of physical health. Though this differentiation is indeed pragmatic, it nevertheless reflects an epistemic position. Even so, further investigation into the very experience of illness is still useful and interesting considering the distinction that is drawn.

Phenomenology
Phenomenology is concerned with the structure of experience (i.e., the first-person point of view experience of an illness) (Fuentes, 2017). A phenomenological perspective is thus particularly useful if one would like to understand what certain illnesses are like, revealing that mental disorders often display extraordinarily bodily features. The unconventional phenomenological approach offers help to understand the distinction drawn between mental and bodily illness, and shines light on the complexity of the matter. The phenomenology of depression provides a good example of phenomenology at work here, in particular Thomas Fuchs’ (2013) phenomenological account.
Depression is generally classified as an affective disorder. As maintained by current psychiatric opinion, its core is constituted by a disturbance of mood and affect, typically connected to negative cognitions, self-evaluations, and emotions such as anxiety, shame, and guilt (American Psychiatric Association, 2013). There are also elective symptoms, such as bodily or vegetative disturbances like loss of appetite, weight, libido, insomnia, and psychomotor inhibition: where the diagnosis receives the supplement ‘with somatic syndrome’ (American Psychiatric Association, 2013). The predominant psychological and psychotherapeutic approaches to depression, however, are based on cognitive (‘mental’) models, and the disorder is considered as a combination of faulty information processing and distorted thinking (Fava et al., 1998). Cognitive Behaviour Therapy (CBT) is usually therefore the recommended treatment (ibid). Notably, whatever the treatment, depression is generally regarded as an ‘inner’ mental and individual disorder. Affective or cognitive symptoms nevertheless are rarely found in all patients suffering from depression, Fuchs (2013) notes. Individuals diagnosed with depression instead might complain of constant fatigue, sickness, numbness, various kinds of joint pain or dysesthesias (an unpleasant feeling of the body when touched) (Fuchs, 2013).

Somatic complaints such as loss of vitality, appetite, and drive, fatigue, sleep disturbances, feelings of pain, burning, tension, numbness or heaviness are in fact found to be more common in depressed patients when consulting the doctor, than depressive mood or guilt feelings (Fuchs, 2013). As cited by Hans-Peter Kapfhammer (2006), Swiss physician and psychiatrist Manfred Bleuler addresses this in his book Depressions in Primary Care:
"It is a common and frequent observation that depressive patients only speak of somatic phenomena while concealing their state of depressive mood. They report palpitations, tightness of the chest, obstipation, pollakiuria, amenorrhea and many others. Only when one looks at their psychic state does one discover that the depression manifests itself not only in the somatic complaints reported, but in various other bodily expressions" (p.228).
Though depression has long been understood as something intrinsically ‘inner’, depressed patients frequently testify completely somatic complaints which may occur alongside or even instead of feelings of guilt and shame typically associated with the mental illness. The point being that, unlike what western psychopathology (Fuchs, 2013) might suggest, a distinction is not so clear cut. Depression, for example, often displays itself through the body. It is less an intra-psychic, but rather a bodily, expressive, interpersonal, or even atmospheric process (Fuchs, 2013).

Phenomenology is especially helpful in recognising this, argues Fuchs (2013), since as a tradition it has an affinity for such concepts and regards the lived body not only as the primary domain of self-experience, of well-being or ill-being, but also as the medium of human elementary contact to the world (Fuchs, 2013). In Fuchs’ (2013) words, “the body is embedded in intercorporeality, and thus becomes the medium of interaffectivity” (p.222). On this view, depression and other so-called ‘mental’ illnesses should preferably be looked on as alterations of the individual’s lived body, lived space, and being-with-others (hence a disturbance of what Fuchs names intercorporeality and interaffectivity). Commonly understood as an ‘inner’ mental disorder, depression is rather like a “detunement” (Fuchs, 2013, p.233) of the lived body that otherwise (normally) connects humans with the social world. Arguably, a distinction drawn between mental and bodily forms of illness is thus untenable if the body plays such a significant role in a mental illness like depression. Notably, treating the body in depression could be a very important tool. Depression as bodily may only be supported by the available evidence concerning the success of physical exercise therapy. This topic, unfortunately, is beyond the scope of this article.
An Untenable Distinction?
Chronic Fatigue Syndrome, otherwise known as Myalgic Encephalomyelitis (hereafter, CFS/ME), further reflects the complexity of drawing a distinction between ‘mental’ and ‘bodily’ forms of illness. CFS/ME is a much-disputed illness that spotlights why a distinction drawn between mental and bodily forms of illness could be untenable, especially if it exacerbates a poor understanding of the illness.
Characterised by persistent fatigue, anxiety, and depression, CFS/ME in the 1980s earned its classification as a non-psychopathological medical disorder, but this has continued to be controversial (Byrne, 2020). Symptoms are quite physical and include disrupted sleep, headaches, a sore throat or sore glands, flu-like symptoms, muscle or joint pain, heart palpitations, and feeling dizzy or sick (Tack, 2019). Some have therefore proposed that CFS/ME should be classified as a ‘functional syndrome’, that is, a syndrome that cannot be explained by an identifiable disease (Tack, 2019). This has also been met with resistance, however, since the term is sometimes associated with an implication of psychogenesis. Others have proposed that CFS/ME ought to be regarded as a neurological disorder that is meaningfully distinct from any psychiatric condition, yet labelling of the disorder generally remains disputed by clinicians, researchers, and patients (Byrne, 2020). What is more, the controversy surrounding CFS/ME has resulted in a dangerous lack of understanding towards the condition, generally amongst the public.

The question of how to treat CFS/ME splits the scientific and patient advocacy communities, becoming the basis of an intense international dispute (Stephenson et al., 2020). It is a good example of how drawing a distinction and labelling illnesses as simply ‘mental’ or ‘physical’ has a significant impact on both general understanding and treatment settings. CFS/ME has its aetiology hotly debated, and though there is evidence that CFS/ME is triggered by certain viruses in some patients and that neurobiological changes such as hypercortisolism (hypercortisolism refers to the clinical state resulting from excessive tissue exposure to cortisol and/or other related glucocorticoids) (Chiodini, 2011) are associated with the syndrome, neither mechanism is sufficient to explain the extent of the symptoms experienced by patients (Moss-Morris et al., 2013).
CFS/ME is a complex illness perhaps best explained in terms of a multifactorial cognitive behavioural model (Moss-Morris et al., 2013) (not simply just a ‘mental’ or ‘bodily’ illness). This model proposes that the illness is precipitated by life events and/or viral illness in vulnerable individuals, such as those who are genetically predisposed, prone to distress, high achievement, and over or under activity (Moss-Morris et al., 2013). Interestingly, treatments based on this model including cognitive behavioural therapy and graded exercise therapy are effective at significantly reducing fatigue and disability in CFS/ME (Moss-Morris et al., 2013). Indeed, both talking-based (psychological) therapy and body-focused treatment is effective in patients diagnosed with CFS/ME (Moss-Morris et al., 2013). Hence drawing a distinction between mental and bodily forms of illness is not a straightforward endeavour. CFS/ME is an example of the kind of illness—like many—which is neither wholly mental nor wholly bodily. Drawing a distinction is questionable having considered the phenomenology of ‘mental’ illness and misunderstood illnesses. It is generally unclear whether evidence can always point to something simply just ‘bodily’ or ‘psychological’ (Stephenson et al., 2020).

Conclusion
According to general consensus, and as the World Health Organisation defines it, (Saracci, 1997) ‘health’ refers to both the physical and mental. General consensus also tends to hold, however, that these are different forms of (ill) health. One must nevertheless question whether a distinction drawn between mental and bodily forms is necessary. Phenomenology, for instance, may show how ‘mental’ disorders such as depression have particularly bodily features. Drawing a distinction is unwarranted if the two forms of illness overlap, and especially if the effects of this are damaging.
This article started by comparing the broad differences between a bodily illness with a mental illness, thus reflecting why a distinction is so often drawn between the two. It then went on to look at the phenomenology of depression, an illness typically understood as ‘mental’ but with exceptionally physical features. The same goes for many mental disorders which often have bodily features on top of ‘inner’ psychological types of symptoms. Fuchs’ (2013) account is thus interesting, suggesting a kind of bodily ‘detunement’ involved with depression and other mental disorders alike. CFS/ME was finally considered. CFS/ME is an unfortunately misunderstood and controversial illness, highlighting an unfeasible distinction as it is an example of yet another illness which is not simply ‘mental’ or ‘bodily’.
Bibliographical References
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Arlington: American Psychiatric Association.
Byrne, E., 2020. Striking the balance with epistemic injustice in healthcare: the case of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Medicine, Health Care and Philosophy, 23(3), pp.371-379.
Chiodini, I. (2011). Diagnosis and treatment of subclinical hypercortisolism. The Journal of Clinical Endocrinology & Metabolism, 96(5), 1223-1236.
Davis, P. B. (2006). Cystic fibrosis since 1938. American Journal of Respiratory and Critical Care Medicine, 173(5), 475–482. https://doi.org/10.1164/rccm.200505-840oe
Fava GA, Rafanelli C, Grandi S, Conti S, Belluardo P. (1998). Prevention of Recurrent Depression With Cognitive Behavioral Therapy: Preliminary Findings. Arch Gen Psychiatry. 1998;55(9):816–820. doi:10.1001/archpsyc.55.9.816
First, M. B., Bhat, V., Adler, D., Dixon, L., Goldman, B., Koh, S., ... & Siris, S. (2014). How do clinicians actually use the Diagnostic and Statistical Manual of Mental Disorders in clinical practice and why we need to know more. The Journal of nervous and mental disease, 202(12), 841-844.
Fuchs, T. 2013. Depression, Intercorporeality and Interaffectivity. Journal of Consciousness Studies 20/7-8: 219-238.
Hardy, S., & Thomas, B. (2012). Mental and physical health comordibity: Political imperatives and practice implications. International Journal of Mental Health Nursing, 21(3), 289-298.
Monjaraz Fuentes, P., Rojas Hernández, M. D. C., Santasilia, S., & Monjaraz Fuentes, F. (2017). The body as constitutive element phenomenology and psychoanalysis on our view of ourselves and others. Life sciences, society and policy, 13(1), 6. https://doi.org/10.1186/s40504-017-0051-0
Kapfhammer, H., 2006. Somatic symptoms in depression. Dialogues in Clinical Neuroscience, 8(2), pp.227-239.
Kendell, R. E. (2001). The distinction between mental and physical illness. The British Journal of Psychiatry, 178(6), 490-493.
Leahy, R. L. (2007). Bipolar disorder: Causes, contexts, and treatments. Journal of Clinical Psychology, 63(5), 417–424. https://doi.org/10.1002/jclp.20360
Moss-Morris, R., Deary, V., & Castell, B. (2013). Chronic fatigue syndrome. Handbook of clinical neurology, 110, 303–314. https://doi.org/10.1016/B978-0-444-52901-5.00025-3
Saracci, R. (1997). The World Health Organisation needs to reconsider its definition of health. Bmj, 314(7091), 1409.
Stephenson, L., Stephenson, L., Howarth, A., Vickers, H., Edwards, M., Edwards, M., Aviram, A., Cable, T. and Raval, P., 2020. Chronic Fatigue Syndrome, Bristol University, And Controversial Science - The Bristol Cable. [online] The Bristol Cable. Available at: <https://thebristolcable.org/2017/07/chronic-fatigue-syndrome-bristol-university-and-controversial-science/> [Accessed 20 December 2020].
Tack M. (2019). Medically Unexplained Symptoms (MUS): Faults and Implications. International journal of environmental research and public health, 16(7), 1247. https://doi.org/10.3390/ijerph16071247
Tang, Y. Y. (2017). The neuroscience of mindfulness meditation: How the body and mind work together to change our behaviour. Springer.
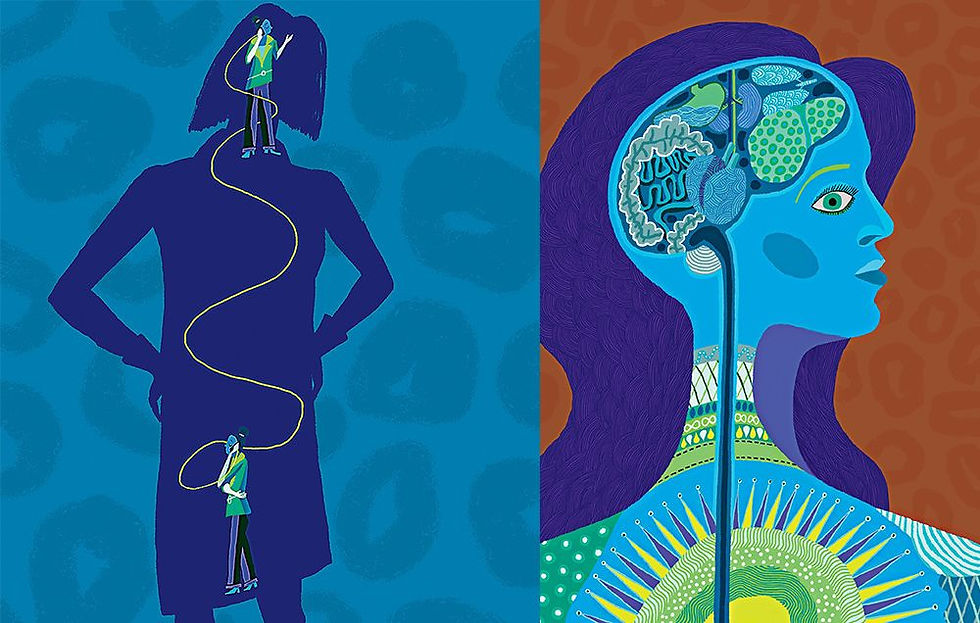
Visual Sources
Cover Image: Cripps, R. (2022). Heart and Mind. The Occupational Therapy Hub. Retrieved January 8, 2023, from https://www.theothub.com/article/mental-and-physical-health-why-they-go-hand-in-hand.
Figure 1: Hart, W. D. 1996. "Dualism." pp. 265–267 in A Companion to the Philosophy of Mind, edited by S. Guttenplan. Oxford: Blackwell.
Figure 2: Tedesco, L. (2018). Mind-body Connection. Women's Health. Retrieved January 6, 2023, from https://www.womenshealthmag.com/health/a18198138/mind-body-connection-illnesses/.
Figure 3: Rare Disease Series: Cystic Fibrosis. (2020). 3 Billion Blog. Retrieved January 6, 2023, from https://3billion.io/blog/rare-disease-series-2-cystic-fibrosis/.
Figure 4: Linden, D. (2019). The Biology of Psychological Disorders. Red Globe Press.
Figure 5: Fuchs, Thomas. (2021). In Defense of the Human Being. Foundational Questions of an Embodied Anthropology. 10.1093/oso/9780192898197.001.0001.
Figure 6: Hardman, I. (2018). Review: The Inflamed Mind: A Radical New Approach To Depression. The Times. Retrieved January 6, 2023, from https://www.thetimes.co.uk/article/review-the-inflamed-mind-a-radical-new-approach-to-depression-by-edward-bullmore-why-doctors-get-mental-health-wrong-7x9b7qk93.
Figure 7: Shan, Z.Y., Kwiatek, R., Burnet, R., Del Fante, P., Staines, D.R., Marshall-Gradisnik, S.M. and Barnden, L.R. (2016), Progressive brain changes in patients with chronic fatigue syndrome: A longitudinal MRI study. J. Magn. Reson. Imaging, 44: 1301-1311. https://doi.org/10.1002/jmri.25283
Figure 8: Common diseases that cause neck pain in adults. (2013). Valley Medical and Wellness. Retrieved January 6, 2023, from https://www.valleymedical.com/blog/common-diseases-that-cause-neck-pain-in-adults-part-1.







Comments